 |
Bios Dr. Feldman is a vitreoretinal surgical fellow at University of California, Davis, Sacramento DISCLOSURES: The authors have no relevant relationships to disclose. |
Perfluorocarbon liquids such as perfluorooctane (PFO) are excellent tools for managing complex retinal detachments.1 PFO has the ability to act as a “third hand” to stabilize the retina, allowing for improved peripheral vitrectomy in cases of highly mobile retina.
However, some surgeons avoid using PFO because they fear complications of subretinal PFO.2 An exceptionally rare complication of PFO in vitreoretinal surgery is entry into the central nervous system. David Malin, MD, and colleagues in 2007 reported one of the first cases involving migration of perfluorocarbon within the intracranial subarachnoid space.3
The intraoperative surprise
In our surgical video, we present a challenging case of a patient undergoing traumatic retinal detachment repair with PFO. This patient had a gunshot wound to the head with multiple orbital wall fractures, but without any apparent open-globe injuries.
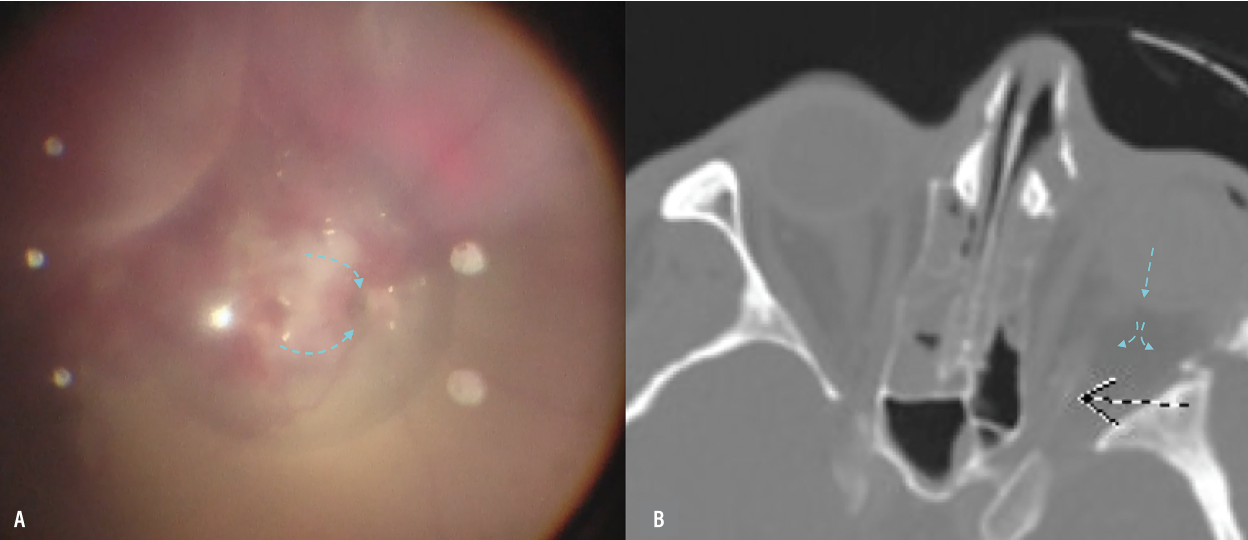
Intraoperatively, we noted a dense vitreous hemorrhage and a complex retinal detachment. After we injected PFO, we surprisingly discovered a small defect near the optic nerve, which allowed the intravitreal PFO to drain out of the eye.
Given that it wasn’t feasible to retrieve the PFO, we made the decision to flatten the retina under air to complete the rest of the case. This choice of tamponade introduced its own challenges in managing this traumatic retinal detachment, but we felt that silicone oil would provide better globe stability over gas and would be less likely to migrate due to the small size of the optic nerve defect. In patients with larger posterior defects, it may be inadvisable to use silicone oil because of the risk of extraocular migration.
 |
|
A) Intraoperative imaging depicts the defect located at the temporal edge of the optic nerve and the route of perfluorooctane (PFO) migration. B) Postoperative computerized tomography scan shows the PFO in the orbit (blue arrows) with possible hyperintensity of the distal optic nerve. |
Postoperative management
Due to our patient’s medical status, we were unable to obtain a postoperative MRI, but the CT scan images demonstrated extraocular migration of PFO with tracking along the optic nerve. These findings supported our belief that an optic nerve avulsion injury was the likely culprit.
Although very rare, the literature has reports of PFO migration into the subarachnoid space.1,4,5 One case reported intraoperative PFO loss and the patient developing sudden systemic decompensation.4 The patient was transferred to an intensive-care unit and the PFO was removed via lumbar puncture.
Our patient didn’t exhibit any ocular or systemic adverse effects of the PFO and maintained good silicone oil fill at postoperative month one. They were, unfortunately, lost to follow-up after they were sent to another hospital.
Bottom line
This case highlights a highly unusual occurrence in a patient with a traumatic retinal detachment in which PFO migrated into the retro-orbital and subarachnoid space due to a small defect near the optic nerve. Retrieving the PFO wasn’t possible, leading to our decision to flatten the retina under air and to leave the patient with silicone oil tamponade for better globe stability.
It’s important to exercise caution when using silicone oil in eyes with larger posterior defects because of the risk of extraocular migration.
Our patient didn’t show any immediate adverse effects, although postoperative follow-up was limited because the patient transferred to another hospital. This case underscores the importance of vigilance during repair of complex cases involving trauma. RS
REFERENCES
1. Coll GE, Chang S, Sun J, Wieland MR, Berrocal MH. Perfluorocarbon liquid in the management of retinal detachment with proliferative vitreoretinopathy. Ophthalmology. 1995;102:630-638; discussion 638-639.
2. Garcia-Valenzuela E, Ito Y, Abrams GW. Risk factors for retention of subretinal perfluorocarbon liquid in vitreoretinal surgery. Retina. 2004;24:746–752.
3. Malin DR, Aulino JM, Recchia FM. Intracranial hyperdense subarachnoid perfluorocarbon droplets after attempted retinal detachment treatment. Emerg Radiol. 2007;14:261-263.
4. Chen L, Zhang Z, Wang Q, Guo Y, Ren B, Ni H. Successful removal of cranial migrated intravitreal perfluorocarbon through a lumbar puncture. J Emerg Crit Care Med. 2020;4:22.
5. Naseripour M, Ghasempour A, Falavarjani KG, Sanjari MS, Yousefi M. Perfluorocarbon liquid migration into the subarachnoid space in a patient with morning glory syndrome. J Curr Ophthalmol. 2015;27:60-62.