|
Bios Dr. Cruz Pimentel is a vitreoretinal fellow at the University of Toronto. |
Patients with recurrent detachments secondary to proliferative vitreoretinopathy (Figure 1) who have already had a vitrectomy with silicone oil tamponade can benefit from vitrectomy under silicone oil.
This technique consists of placing all three trocars to allow the peeling and removal of membranes without removing the silicone oil. Different terminology has been used to describe this technique. We’ve previously described this as the silicone sandwich technique.
As a modification of the original interface vitrectomy technique, instead of placing two trocars, cannula and fluid-silicone drainage, we prefer to place three trocars and use the infusion connected to air but clamped, as Peter Kertes, MD, and Gholam Peyman, MD, described in 19971 and Tarun Sharma, MD, in 2002.2
Achieving drainage
You can achieve drainage of the subretinal fluid by increasing the pressure of the infusion connected to air. The efflux of subretinal fluid can be boosted and a combination of passive and active drainage of subretinal fluid can be used.1,2,
After trocars are placed, the silicone oil can act as a third hand for peeling the membranes tangentially. It’s important to note that the appearance of the retina and the membranes under silicone oil are different than when viewed under fluid. Take caution to avoid iatrogenic breaks by carefully grasping and remaining tangential to the retina.
Diathermy can be used to mark the breaks, and drainage of the subretinal fluid can best be achieved by using active fluid extrusion with a blunt tip cannula. At this step, it’s essential to unclamp the air infusion using a snap, which allows the air to go in and promotes more complete fluid drainage, because this increases intraocular pressure and pushes the retina back into place. The air bubble enhances visualization.2,3 Alternatively, the drainage can be done without using the air, and with just using the silicone oil as the infusion and topping up as you go to keep the eye inflated.
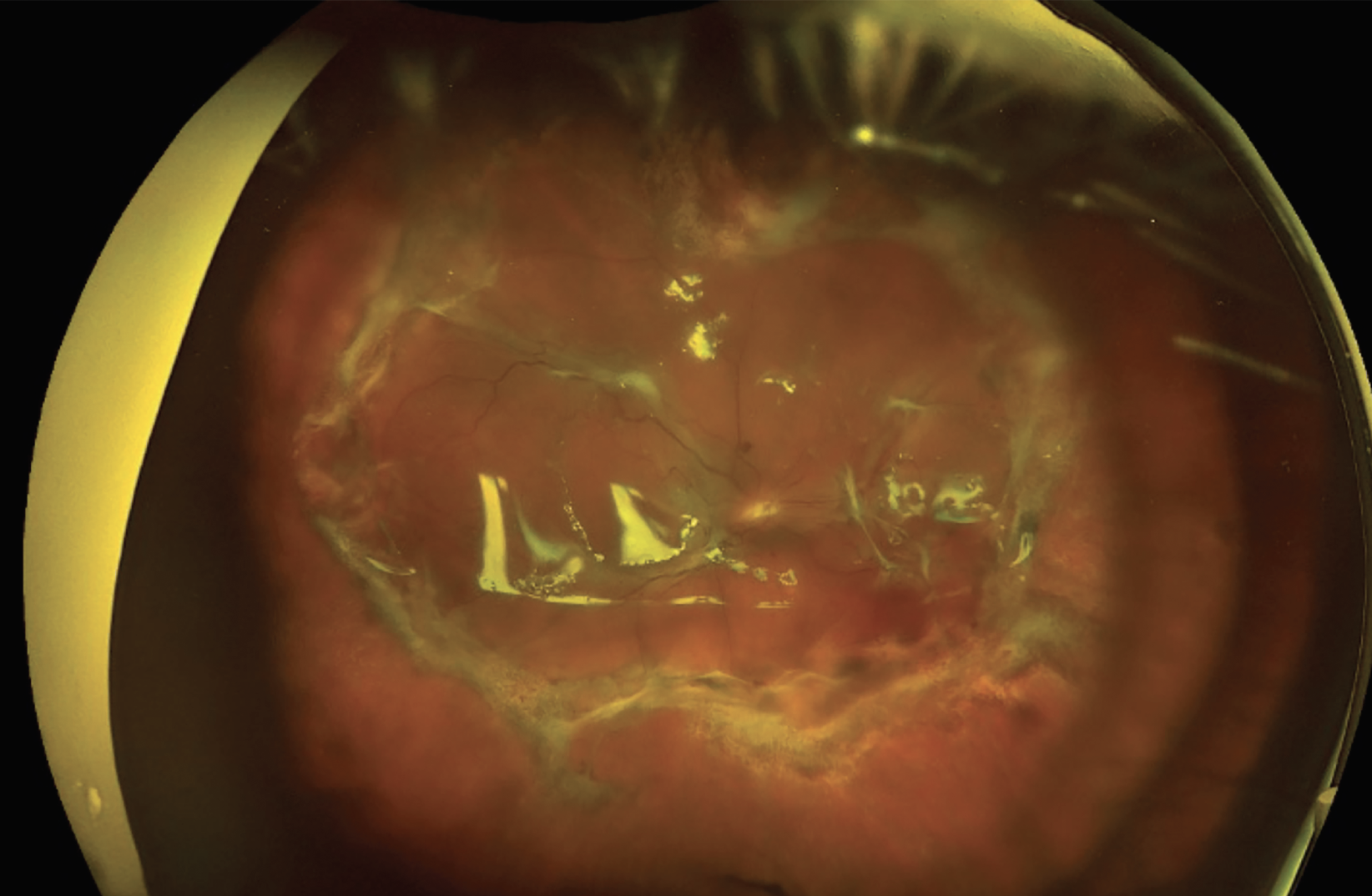 |
| Figure 1. A recurrent retinal detachment secondary to proliferative vitreoretinopathy before surgery. |
With retinal reattachment, laser retinopexy can be applied, and the laser can also be used to help ascertain if the subretinal fluid has been drained adequately.
At the end of the surgery, vent the air, reduce the air infusion pressure and supplement the silicone oil fill because some silicone is always lost during the surgery due to inserting and removing the instruments, removing membranes and draining the subretinal fluid (Figure 2). We believe that this technique works because infusing air pushes silicon oil onto the retinal surface, creating more tension, which allows for drainage.
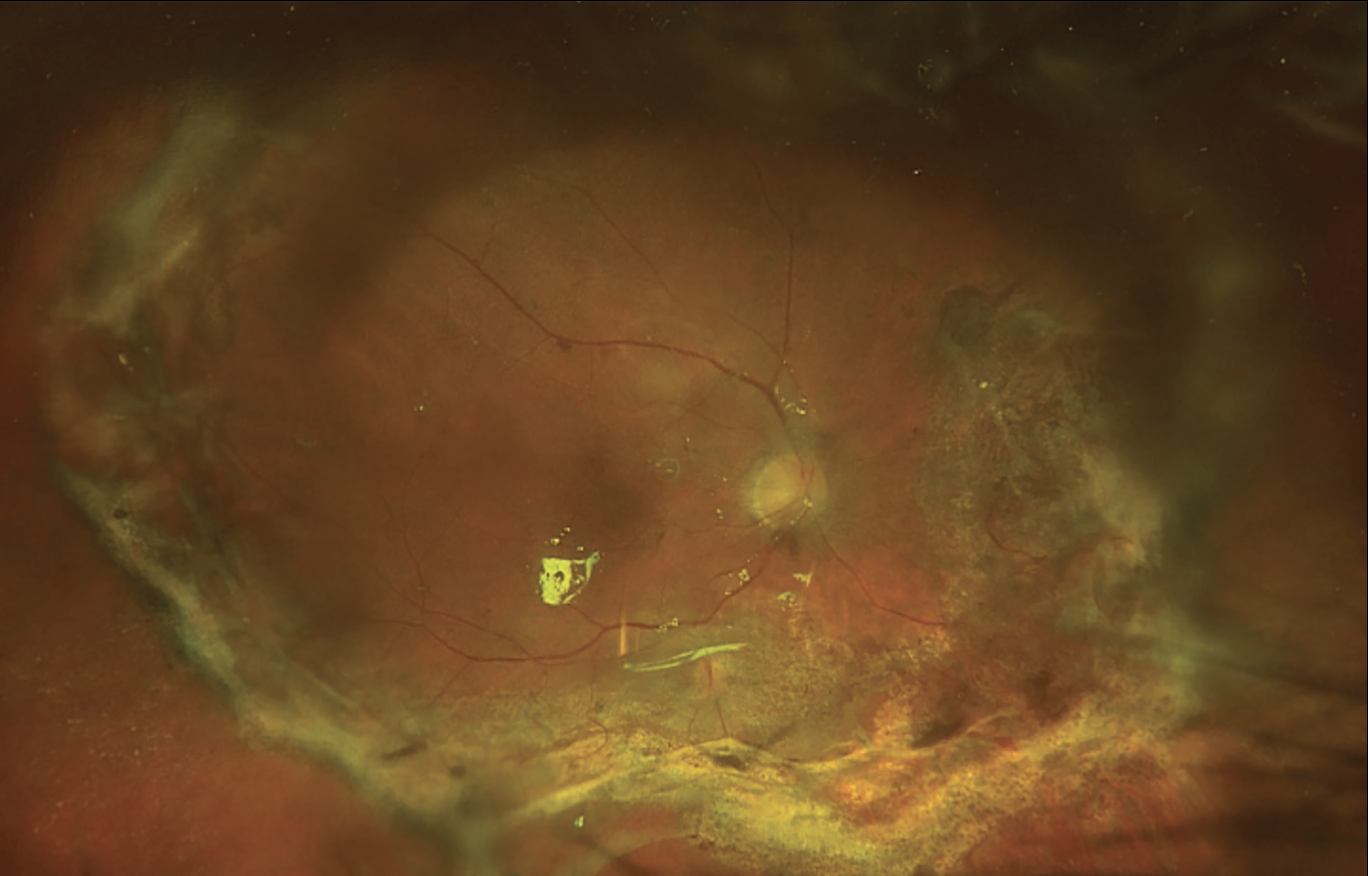 |
| Figure 2. The same recurrent retinal detachment from Fig. 1, secondary to proliferative vitreoretinopathy after surgery. |
Timing of surgery
The timing of this surgery is important and a key to its success. It’s best to intervene only when the PVR is significant enough to easily see and peel. This will ensure that the traction that’s present can be relieved and the retina reattached. In some cases, despite peeling all that can be seen, the retina remains foreshortened and a relaxing retinotomy is necessary.
Bottom line
This technique has many advantages.3 It can be done efficiently and minimizes undue manipulation of the retina. It rarely causes progression of the detachment that’s present in the same way that removal and replacement of the silicone oil would. As a result, this too will limit liberation of retinal pigment epithelium cells and decrease the risk of recurrent PVR and recurrent detachment. RS
REFERENCES
1. Kertes PJ, Peyman GA. Drainage of subretinal fluid under silicone oil. Can J Ophthalmol. 1997;32:445-446.
2. Sharma T, Gopal L, Shanmugam MP, et al. Management of recurrent retinal detachment in silicone oil-filled eyes. Retina. 2002;22:153-157.
3. Yang CM, Hsieh YT, Yang CH, Liu KR. Irrigation-free vitreoretinal surgery for recurrent retinal detachment in silicone oil-filled eyes. Eye (Lond). 2006;20:1379-1382.