Take-home points
|
 |
Bios Dr. Reddy is a consultant ophthalmologist at L.V. Prasad Eye Institute in Hyderabad, India. Dr. Tyagi is head, Smt. Kanuri Santhamma Centre for Vitreo-Retinal Diseases at the Kallam Anji Reddy Campus in Hyderabad. DISCLOSURES: Dr. Reddy and Dr. Tyagi have no relevant disclosures. |
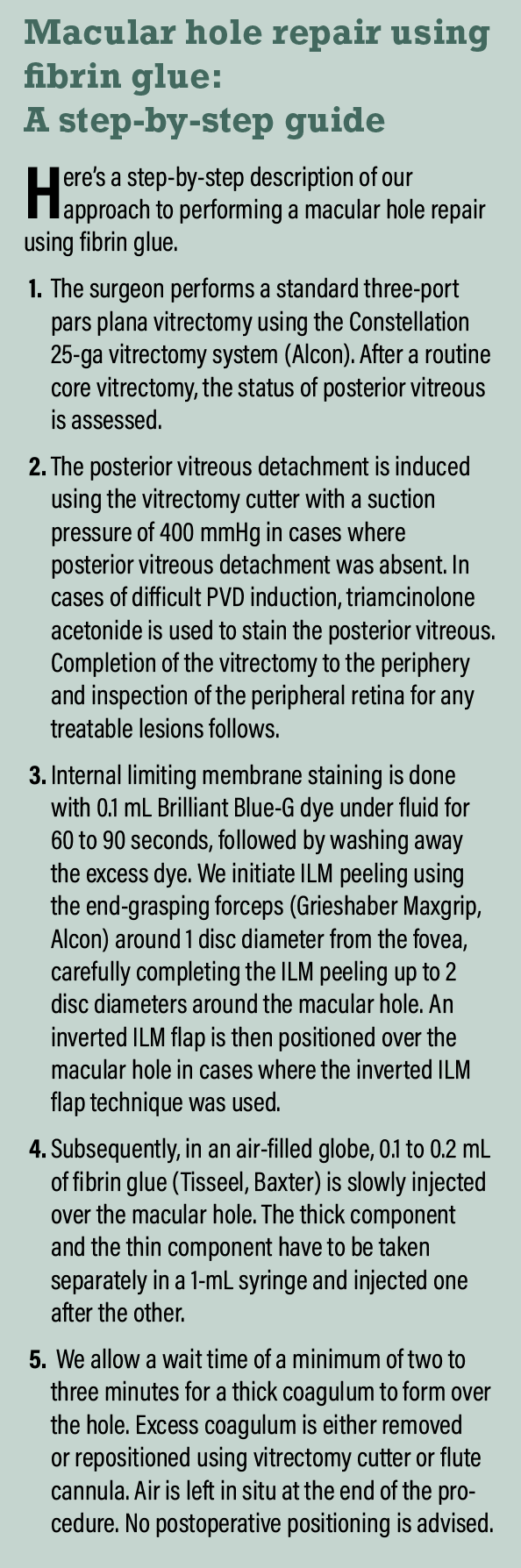
Surgical management of macular holes has undergone significant changes in the last few decades. The aim of surgery is to reduce the anteroposterior traction with the help of vitrectomy and eliminate tangential traction by using internal limiting membrane peeling for stage 3 and 4 macular holes.
While simple pars plana vitrectomy alone has a closure rate of around 58 percent,1 the addition of ILM peeling has resulted in closure rates of 96 to 100 percent, depending upon different sizes of MH.2-4 Over the years, several modifications to MH surgery have evolved, including the use of autologous ILM flaps, inverted ILM flap, temporal ILM flaps and autologous neurosensory retinal free flaps.5,6
The current protocol for macular hole management requires the filling of the vitreous cavity with air or gas along with postoperative prone positioning. Although no consensus exists for the duration of prone positioning, patients are usually advised to do so for one to two weeks. This can be undesirable and distressing for some patients. Also, it might become extremely inconvenient if a patient can’t lie prone due to old age or spinal problems, or if the patient is planning for air travel.
According to the GuARD study, by our group, fibrin glue, which is a biological tissue adhesive composed of thrombin and fibrinogen, can be used as a temporary tamponading agent for rhegmatogenous retinal detachments to avoid postoperative positioning.7,8 This study also found that fibrin glue is efficient and safe as an ocular tissue sealant.
In this study, we proposed a technique of ILM peeling along with application of fibrin glue over the hole. We hypothesized that this would obviate the need for postoperative prone positioning and also avoid use of the conventional gas tamponade.
Alternative to face-down positioning?
Gas or air acts as a scaffold over the macular hole for glial proliferation, and its surface tension tends to extrude the subretinal fluid around the hole.9 This often requires postoperative prone positioning for prolonged duration.10
Although reports have suggested that a prone position is not often necessary for a successful closure of macular hole,11-14 they’ve been met with much controversy owing to the fact that they didn’t consider the duration of hole prior to surgery, with fresh and short-duration holes usually not requiring face-down positioning.
 |
Nonetheless, a meta-analysis showed that prone positioning is often necessary for eyes with hole diameter >400 µm.14 However, several challenges are associated with postoperative prone positioning or the use of gas tamponade. First, maintaining the position depends on patient compliance. It can be especially difficult for older patients and patients with obesity and spinal problems.
Second, problems associated with gas tamponade, such as avoiding air travel and risk of raised intraocular pressure and cataract formation, also need to be considered.15 While air may also expand, it gets absorbed faster than intraocular gases, so its use can reduce the time for which air travel is restricted.
We don’t use intraocular gas in any of our patients. Neither do we advise postoperative prone positioning. We hypothesize that the fibrin glue over the macular hole helps prevent entry of fluid into the hole, and its contraction postoperatively may lead to apposition of hole edges resulting in closure. Also, inclusion of an inverted ILM flap over the hole was done in a few of our cases, and it may act as an additional scaffold to aid in closure.
GuARD study findings
In our study,7,8 we demonstrated the use of fibrin glue as an alternative to gas tamponade for macular hole closure. Our results showed a favorable outcome with the technique as a majority of eyes demonstrated structural closure and visual acuity improvement without the need for postoperative prone positioning.
 |
|
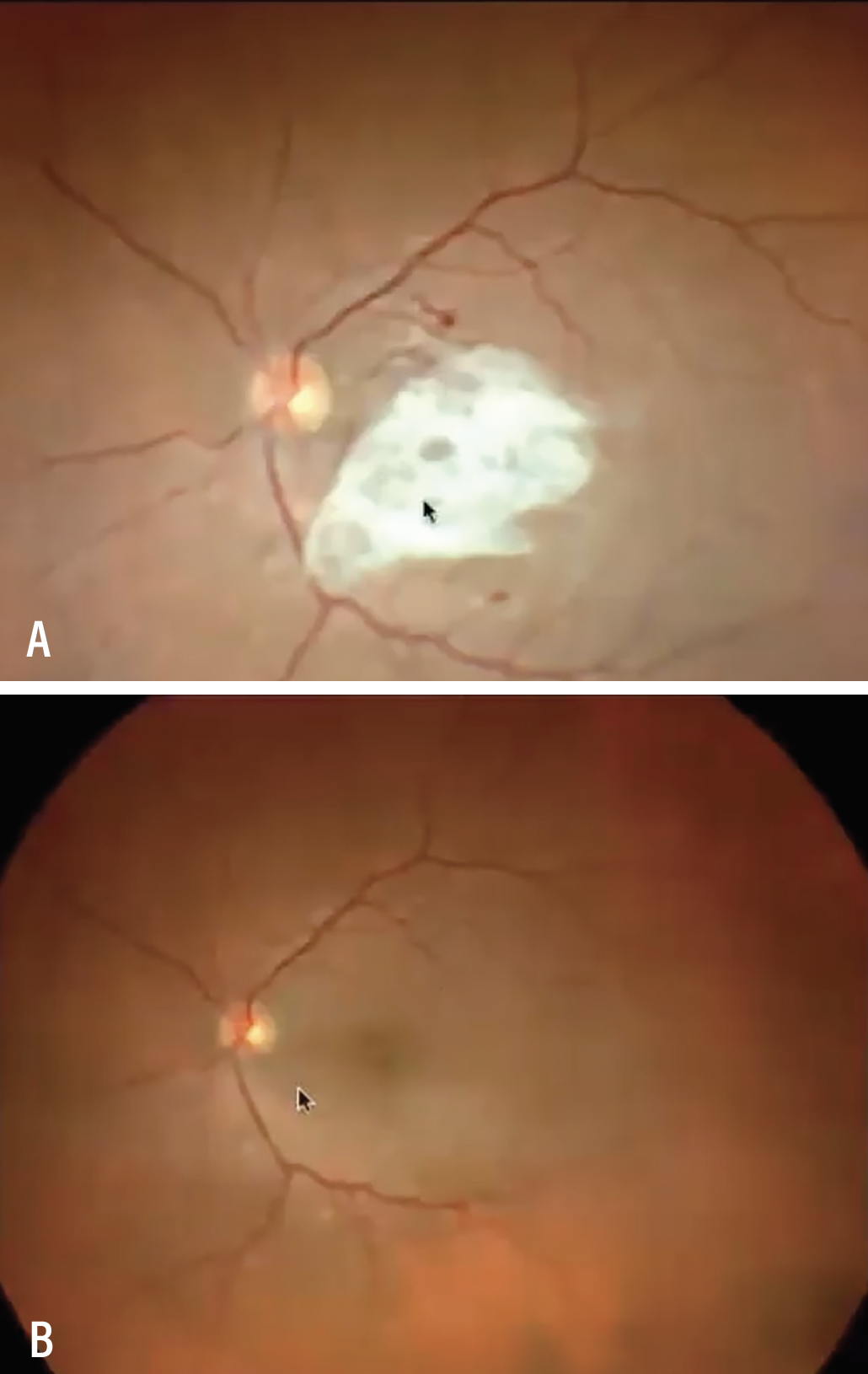
A) At day one postoperatively, the fibrin coagulum was present over the macular area. B) A week later, it was completely resorbed. |
Eight of 10 cases had a complete type 1 closure of the macular hole. We noted the fibrin coagulum was present over the macular area at day one postoperative (Figure A) and was completely resorbed by the one-week visit (Figure B). Two failed cases underwent a repeat surgery with fluid gas exchange and a successful type 1 closure was achieved after the fluid-gas exchange.
One of the failed cases had an inverted ILM flap, which became displaced during the glue application. The ILM was repositioned and fluid-gas exchange was done during the second surgery,
 |
Concerns about fibrin glue
One of the concerns about the use of fibrin glue is the possibility of intraocular inflammation. While the glue has been extensively used in anterior segment surgeries, such as pterygium, amniotic membrane and Tenon patch grafting, its intraocular use has rarely been described, although there have been reports of intraocular fibrin glue use in the management of uncomplicated retinal detachment with good anatomical outcomes.7
Our group also demonstrated its favorable long-term outcome and safety, with no eyes developing raised IOP or intraocular inflammation.8 This makes fibrin glue an attractive alternative for macular hole surgery.
One of the most important aspects about using intravitreal fibrin glue is the mode of application. Although the commercially available glues come with an injector, we think it’s better to avoid its use because it might block the 25-ga flute cannula. The thick component and the thin component have to be taken separately in a 1-mL syringe and injected one after the other. We advise injecting the thick component first because the thin component may spread over an area larger than intended. Any excess coagulum can be repositioned or trimmed with the help of a vitrectomy cutter.
Bottom line
In our experience, we’ve had good anatomical and functional outcomes after glue-assisted macular hole surgery, without the need of a prone positioning or gas tamponade. RS
REFERENCES
1. Kelly NE, Wendel RT. Vitreous surgery for idiopathic macular holes: Results of a pilot study. Arch Ophthalmol. 1991;109:654-659.
2. Tewari A, Almony A, Shah GK. Macular hole closure with triamcinolone-assisted internal limiting membrane peeling. Retina. 2008;28:1276-1279.
3. Sakaguchi H, Ohji M, Oshima Y, Ikuno Y, Gomi F, Maeda N, et al. Long-term follow-up after vitrectomy to treat idiopathic full-thickness macular holes: Visual acuity and macular complications. Clin Ophthalmol. (Auckland, NZ). 2012;6:1281-1286.
4. Jordan F, Jentsch S, Augsten R, Strobel J, Dawczynski J. Study on the time course of macular pigment density measurement in patients with a macular hole—clinical course and impact of surgery. [Article in German] Klin Monbl Augenheilkd. 2012;229:1124-1129.
5. Michalewska Z, Michalewski J, Dulczewska-Cichecka K, Adelman RA, Nawrocki J. Temporal inverted internal limiting membrane flap technique versus classic inverted internal limiting membrane flap technique: A comparative study. Retina. 2015;35:1844-1850.
6. Michalewska Z, Michalewski J, Adelman RA, Nawrocki J. Inverted internal limiting membrane flap technique for large macular holes. Ophthalmology. 2010;117:2018-2025.
7. Tyagi M, Basu S. Glue-assisted retinopexy for rhegmatogenous retinal detachments (GuARD): A novel surgical technique for closing retinal breaks. Indian J Ophthalmol. 2019;67:677-680.
8. Tyagi M, Pappuru RR. Glue assisted retinopexy for rhegmatogenous retinal detachments: GuARD study: Long term outcomes of a new surgical technique. Invest Ophthalmol Visual Science. 2020;61:3707.
9. Xirou T, Theodossiadis PG, Apostolopoulos M, et al. Macular hole surgery with short-acting gas and short-duration face-down positioning. Clin Ophthalmol. 2012;6:1107.
10. Thompson JT, Smiddy WE, Glaser BM, Sjaarda RN, Flynn Jr HW. Intraocular tamponade duration and success of macular hole surgery. Retina. 1996;16:373-382.
11. Tornambe PE, Poliner LS, Grote K. Macular hole surgery without face-down positioning. A pilot study. Retina. 1997;17:179-185.
12. Yagi F, Sato Y, Takagi S, Tomita G. Idiopathic macular hole vitrectomy without postoperative face-down positioning. Jpn J Ophthalmol. 2009;53:215-218.
13. Carvounis PE, Kopel AC, Kuhl DP, Heffez J, Pepple K, Holz ER. 25-gauge vitrectomy using sulfur hexafluoride and no prone positioning for repair of macular holes. Retina. 2008;28:1188-1192.
14. Hu Z, Xie P, Ding Y, Zheng X, Yuan D, Liu Q. Face‐down or no face‐down posturing following macular hole surgery: A meta‐analysis. Acta Ophthalmologica. 2016;94:326-333.
15. Kanclerz P, Grzybowski A. Complications associated with the use of expandable gases in vitrectomy. J Ophthalmol. 2018 :8606494.



