 |
Bios Dr. Cruz Pimentel is a vitreoretinal fellow at the University of Toronto. Dr. Felfeli is an ophthalmology resident at the University of Toronto. Dr. Mandelcorn is a vitreoretinal surgeon at the University of Toronto. DISCLOSURES: The authors have no relevant disclosures. |
Taut neovascular fibrotic membrane caused by regressed neovascularization is common in patients with tractional retinal detachment.1 Retinal fibrosis can be present in two variations, fibrovascular and avascular.
Müller cells play an essential role in the development of retinal fibrosis. As a response to chronic stress, these cells undergo massive gliosis.1,2 When neovascularization is located near the fovea,3 there’s a risk of intraoperative deroofing of the fovea, leading to a macular hole with irregular edges.
In such cases, attempting an internal limiting membrane peel with or without an inverted flap is always a good option. However, peeling the ILM can be difficult because of subretinal fluid in long-standing retinal detachment. An amniotic
membrane could be an alternative, but it may not be readily available in the operating room during the complication.
A retina autograft may also be an alternative, but it requires creation of a second retinal break in an eye that has active proliferation, which can lead to recurrent retinal detachment and proliferative vitreoretinopathy.
Our case
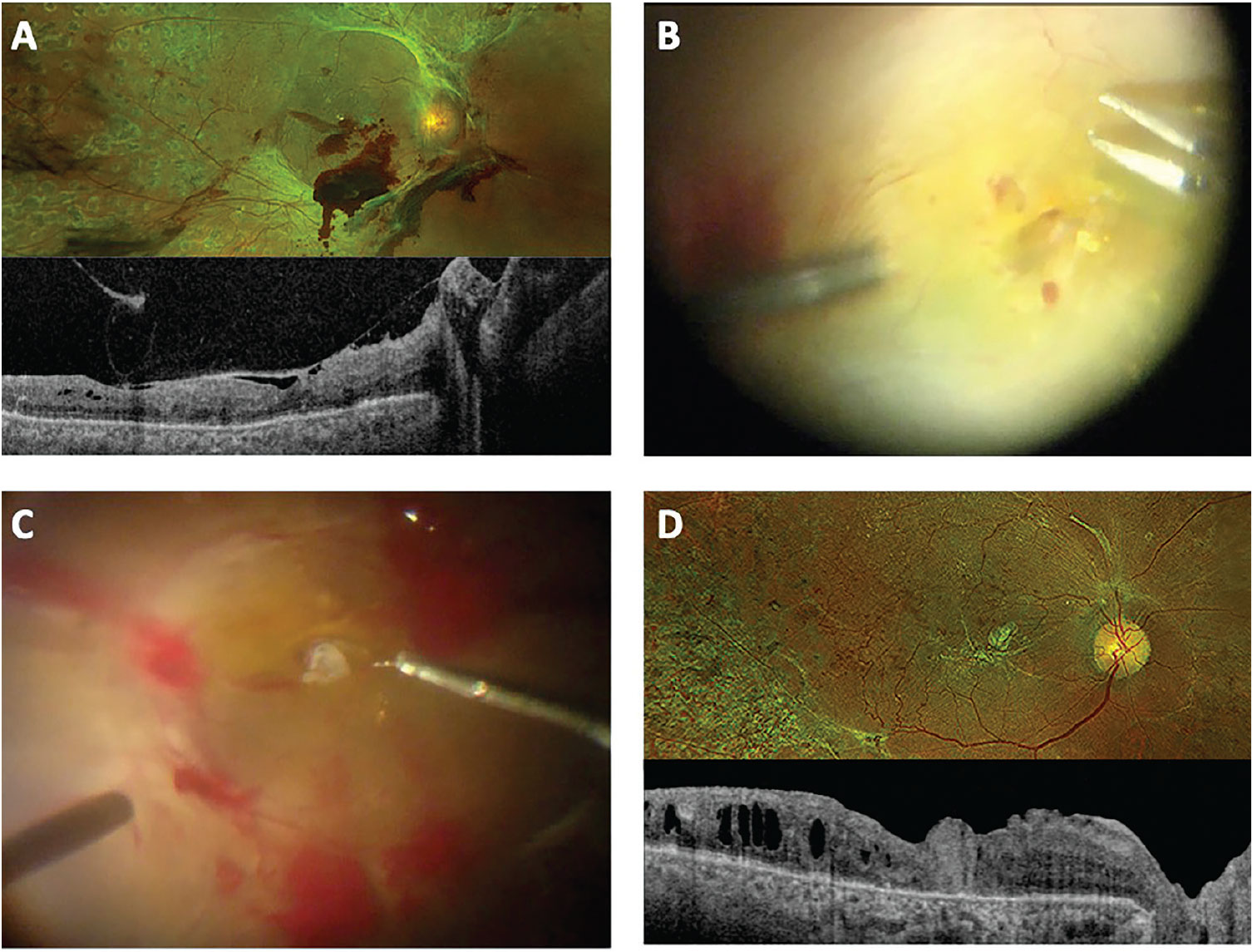
In this case, a 60-year-old female with type 2 diabetes presented with a complex tractional diabetic retinal detachment in the right eye. We advised surgery, but the patient didn’t return for three months, and the TRD worsened. Visual acuity had deteriorated to hand motion.
Intraoperatively, while removing foveal attachments of regressed fibrotic tissue, we noted a macular tear with ragged edges caused by deroofing of the fovea during surgery.
We made an initial attempt to peel the ILM, but subretinal fluid and complex exudates made creating an ILM-inverted flap impossible. We deliberately left a residual patch of regressed retinal fibrosis without delamination prior the fluid-air exchange to serve as a macular plug.
After completing the removal of the peripheral vitreous, and using ILM forceps to delicately dislodge the fibrosis patch, which was deliberately left tethered at its attachment site, we placed this fibrotic neovascular patch to plug the macular tear. Postoperatively, the patient had a complete macular hole closure without central scotoma. Visual acuity was 20/400 at the two-month follow-up.
 |
|
A) Preoperative optical coherence tomography of a patient with complex tractional diabetic retinal detachment in the right eye. B) A large intraoperative macular tear was inadvertently created while removing foveal attachments of regressed fibrotic tissue. C) A patch of regressed retinal fibrosis was used as a graft to plug the macular tear. D) At two months postoperatively, the patient had relatively good anatomical and functional outcomes with complete macular hole closure without a central scotoma and a visual acuity of 20/400. |
Bottom line
This case highlights the use of regressed neovascular tissue as a solution for intraoperative management of macular holes caused by deroofing during TRD surgery. In cases where an unanticipated macular hole forms and no prepared amniotic membrane graft is available to close the macular tear, fibrotic neovascular membranes can be used to achieve anatomical closure. RS
REFERENCES
1. Roy S, Amin S, Roy S. Retinal fibrosis in diabetic retinopathy. Exp Eye Res. 2016;142:71-75.
2. Bringmann A, Reichenbach A. Role of Muller cells in retinal degenerations. Front Biosci. 2001;6:E72-E92.
3. Seth A, Ghosh B, Bhambhwani V, Gupta A, Raina UK. Foveal neovascularization in a patient with type 2 diabetes mellitus. Oman J Ophthalmol. 2017;10:255-256.




