 |
|
Bio Ananth Sastry, MD is an attending surgeon and faculty member of the Vitreoretinal Service at the Cleveland Clinic Cole Eye Institute. Disclosures: Dr. Sastry is a consultant to Allergan, Bausch + Lomb, and Genentech/Roche. |
Ocular inflammatory diseases present several challenges to the clinician. These patients often have complicated histories, can be difficult to examine and the underlying diseases may rapidly become vision- or even life-threatening. However, with an organized and methodical approach, even the most complex or mysterious cases can be successfully diagnosed and managed. Here, I’ll discuss five pieces of data that can be obtained from the history and physical and can be used to generate a focused differential that can streamline your work-up and management. They can also help avoid pitfalls such as ordering an excessive number of tests or starting patients on inappropriate treatment.
1. What are the patient’s demographics?
As medical students, we all learn that the best doctors are the ones who can diagnose the patient as soon as he or she walks in. This is sometimes achievable in uveitis, as the patient’s demographics may narrow down the differential before the eye exam.
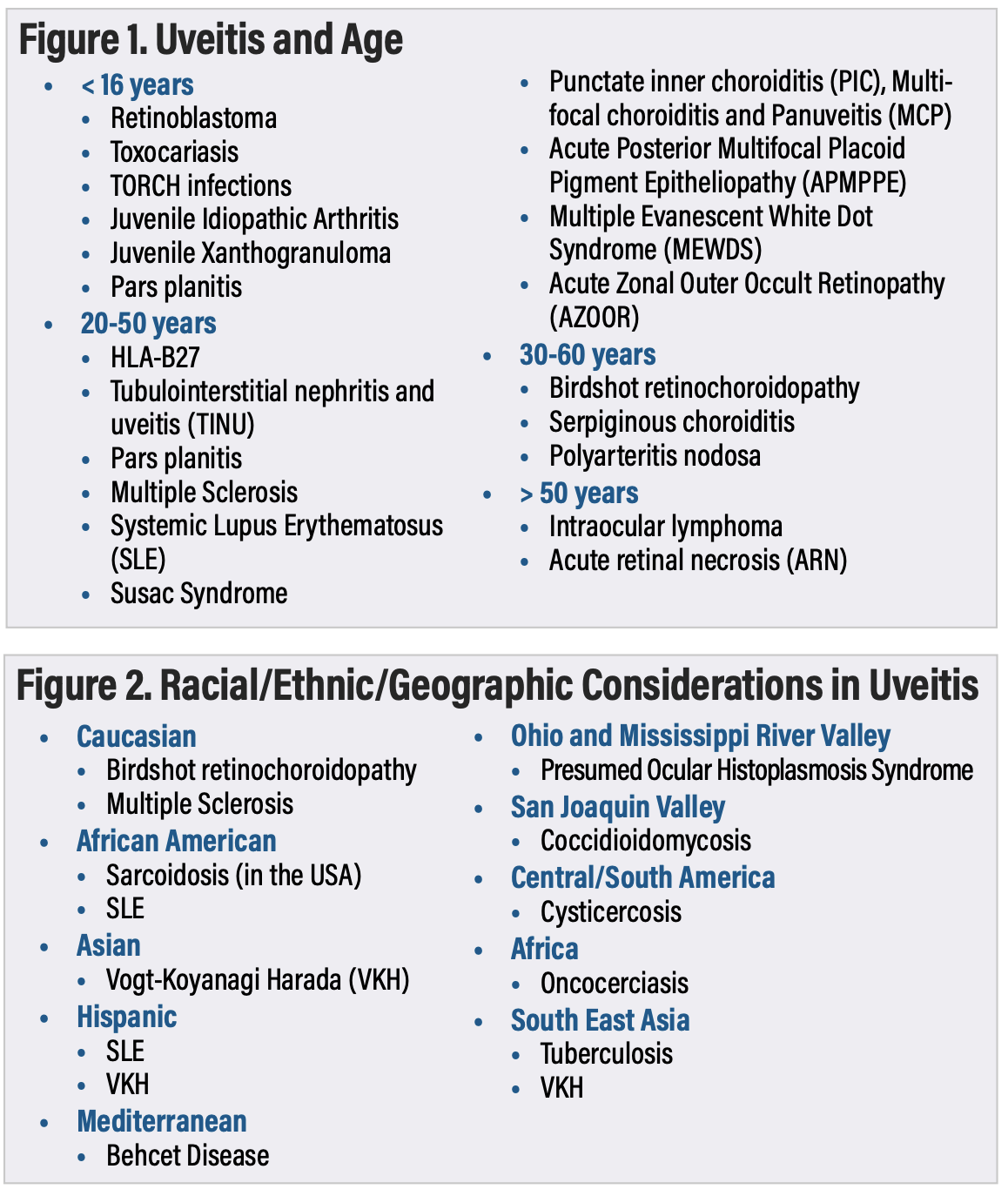
• Age. The majority of patients with uveitis are between 20 and 60 years old.1 However, certain types of uveitis are far more likely in particular age groups (Figure 1). For instance, one would not be tempted to include intraocular lymphoma high on the differential in a 23-year-old immunocompetent patient. Similarly, it would be unlikely for a 62-year-old patient to develop an acute onset of toxocariasis-related uveitis.
 |
• Sex. While most ocular inflammatory diseases affect males and females equally, there are several that have a predilection for females such as multiple sclerosis, lupus, Susac syndrome and most of the white dot syndromes.
• Race/ethnicity/geography. The patient’s race or ethnicity may predispose him or her to certain types of uveitis. For instance, birdshot chorioretinitis is seen almost exclusively in Caucasians. Sarcoidosis is more prevalent in African Americans and patients of Northern European descent, but less common in Asians. Additionally, a patient’s presence within certain geographic locations may make him or her more vulnerable to certain endemic infectious diseases (Figure 2).
 |
2. What is the timing/chronicity of the inflammation?
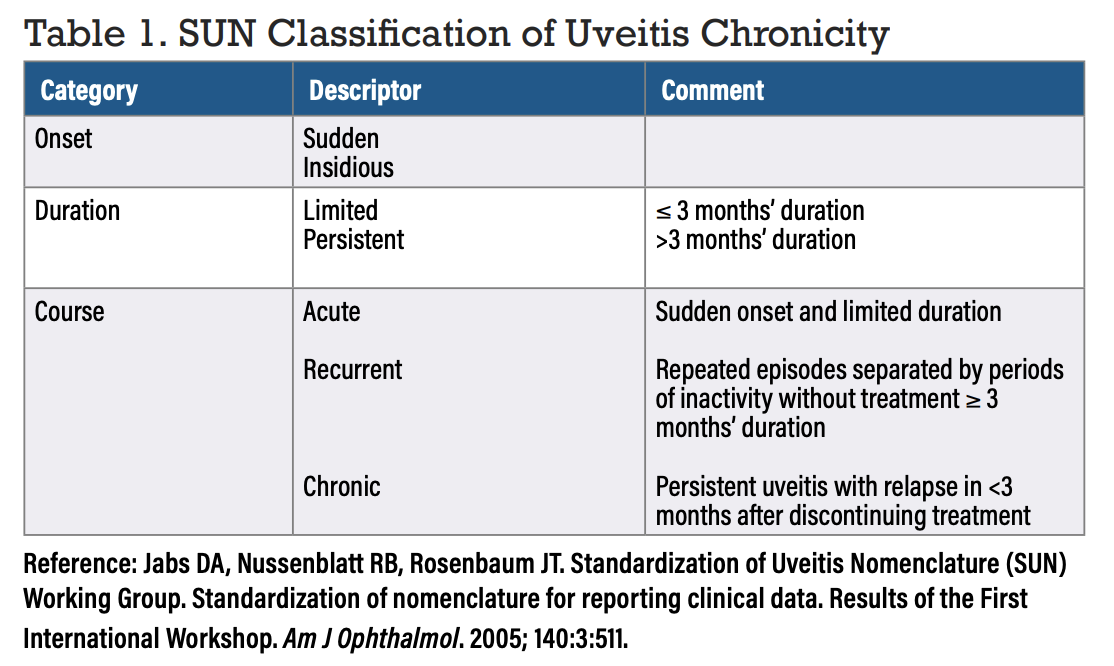
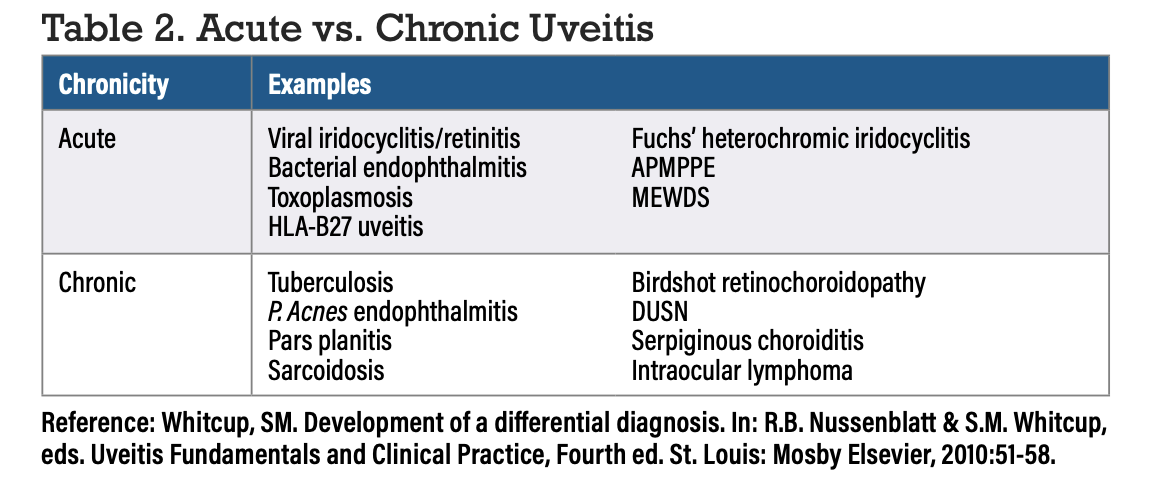
The standardization of uveitis nomenclature (SUN) working group helped to sort uveitis into various categories, one of which involved the temporal aspects of the disease in terms of onset, duration and course (Table 1).2 These temporal distinctions are useful when narrowing the differential, as different diseases operate at various speeds (Table 2).
 |
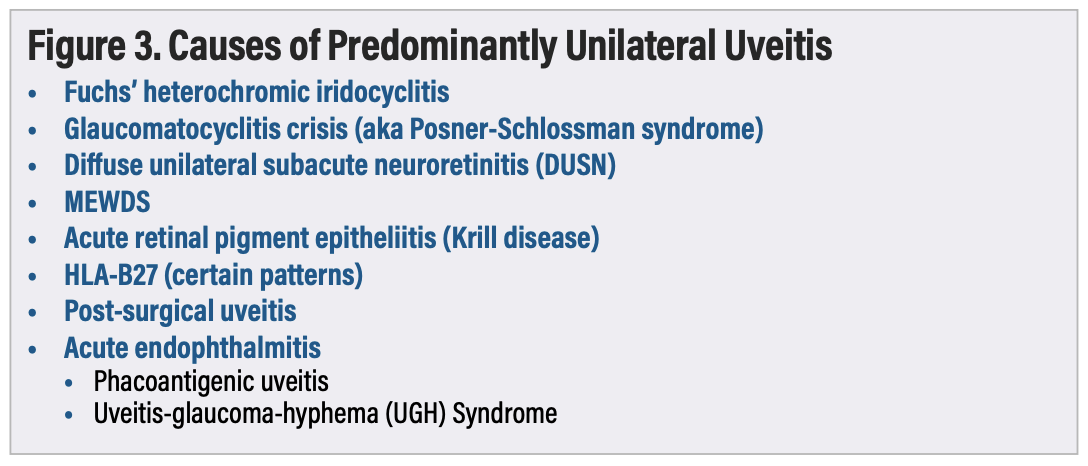
3. Is the pathology unilateral or bilateral?
Most forms of uveitis are ultimately bilateral even if they’re very asymmetric or take an extended period of time for the fellow eye to become involved. Thus, knowledge of the handful of uveitis conditions that are predominantly unilateral (Figure 3) may help arrive at the diagnosis.
 |
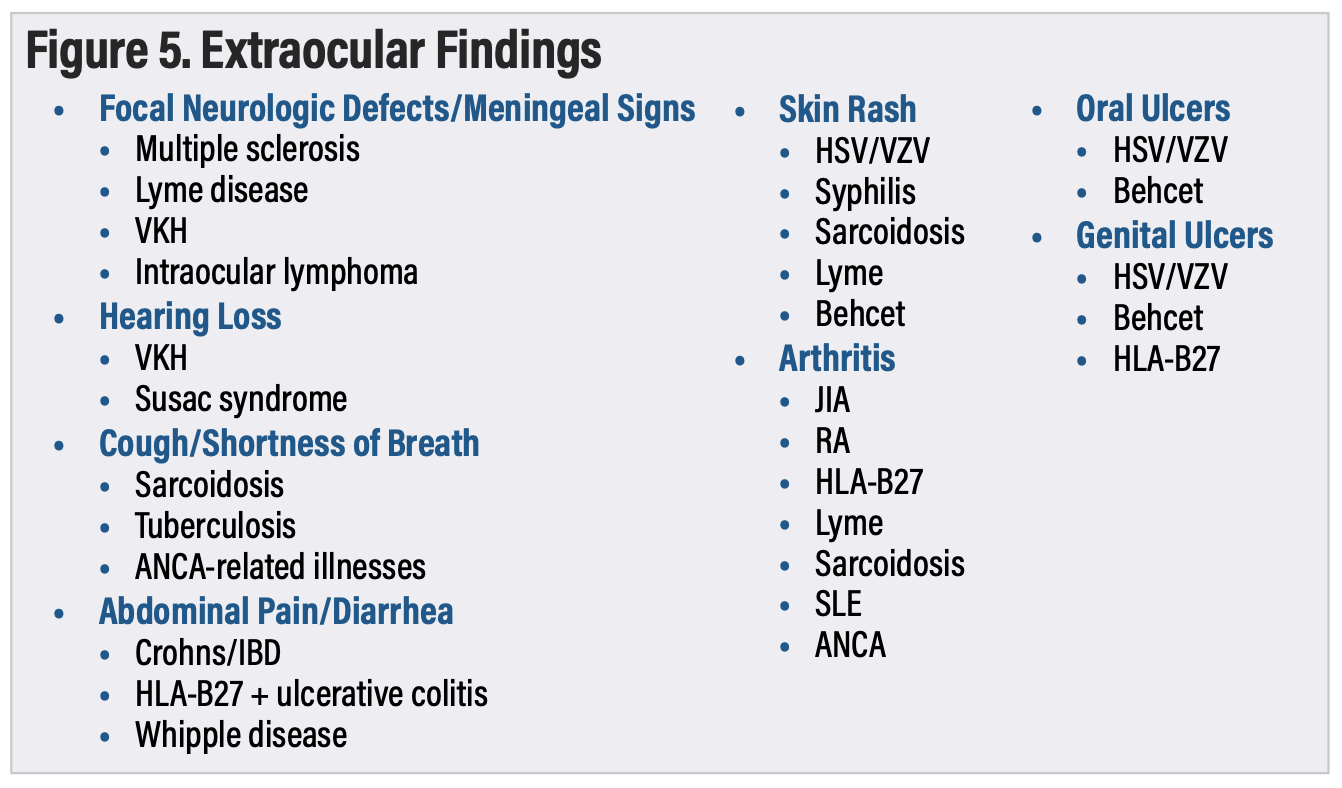
4. What are the associated systemic symptoms or findings?
While it can be time-consuming, performing a detailed review of systems is absolutely critical when evaluating uveitis patients. Because uveitis often involves conditions that affect multiple organ systems, this is important not only for reaching a diagnosis, but also to identify conditions that may be life-threatening and need to be addressed immediately.
 |
| Figure 4. Maculo-papular rash in a patient with bilateral panuveitis secondary to syphilis. |
In my experience, it’s not adequate to simply ask the patient in an open-ended manner if they have any other symptoms outside of the eye. Patients frequently leave out important associated findings because they forget, don’t think they’re important, or are embarrassed to talk about them. They may initially deny having any other symptoms, but later when asked about specific symptoms such as a rash (Figure 4) or joint pain, they will reveal findings that they had previously omitted. Figure 5 demonstrates a list of symptoms that can be associated with specific diagnoses.
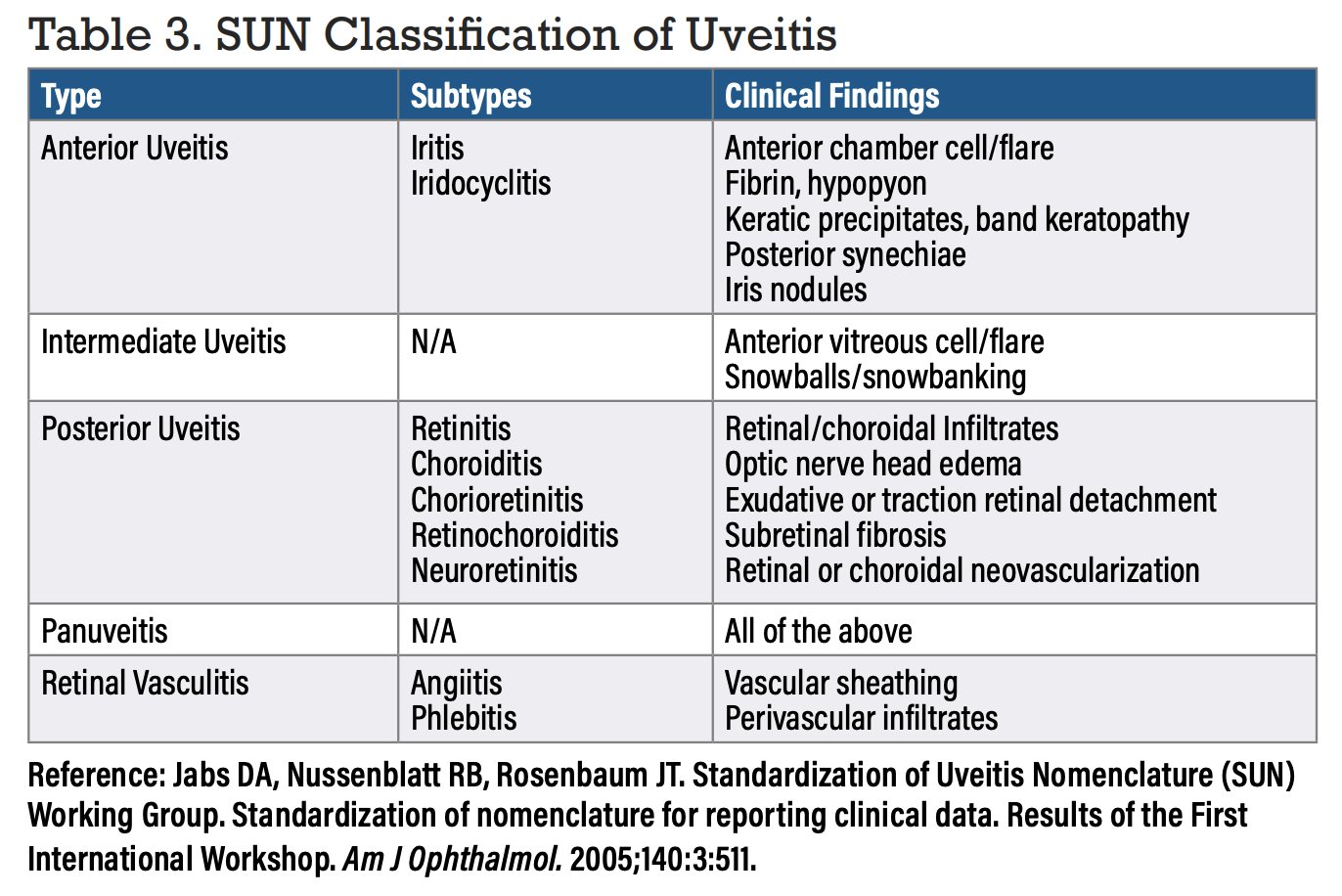
5. Where is the inflammation located?
To say that a patient has “uveitis” is as descriptive as saying that a patient has a “retina problem.” For this reason, the SUN classification system is useful in categorizing uveitis based on the location of the inflammation (Table 3). This method of precisely describing uveitis based on localization can greatly focus down the differential. When evaluating patients, I find that many ophthalmologists aren’t sufficiently familiar with the classification and end up labeling cases of intermediate uveitis or retinal vasculitis as “posterior uveitis” or describing posterior uveitis as “panuveitis.”
Performing a thorough ophthalmic exam including the ocular surface and adnexa is critical to correctly localize inflammation. For instance, it’s important to always check under the lids, which can reveal clues such as salmon patches secondary to lymphoma or an inflamed lacrimal gland from sarcoidosis. The anterior vitreous should be examined with a 1 x 1 slit beam to check for cell, not just the anterior chamber. Additionally, the far inferior retinal periphery should be checked to evaluate for snowbanking. Sometimes scleral depression is required to visualize this.
 |
 |
Putting it all together
Imagine you have three patients who have been referred to you. You’re told one has anterior uveitis, the second has vitritis, and the third has panuveitis. Do you have a good sense of your diagnosis and plan for these patients with the information provided? What if we were to add each of the pieces of data described above to these scenarios?
• Now the first patient is a 28-year-old Caucasian male who presents with an acute, unilateral iridocyclitis with concurrent lower back pain.
• The second patient is a 37-year-old African female presenting with chronic, unilateral intermediate uveitis. Review of systems is positive for circular skin lesions on her shins.
• The third patient is a 43-year-old female from India presenting with acute, bilateral panuveitis. She notes that several weeks prior to her vision changes, she suffered from fever, neck stiffness and hearing loss.
With the addition of just five pieces of data for each of these cases, the clinician is guided almost directly to the diagnoses.
Bottom Line
When working up uveitis, assess the patient’s demographics, take a detailed history with emphasis on chronicity and laterality, perform a detailed review of systems, determine the location of the inflammation and use the SUN classification. This organized approach may help improve efficiency and diagnostic accuracy. RS
REFERENCES
1. Whitcup, SM. Development of a differential diagnosis. In: Nussenblatt RB and Whitcup SM, eds. Uveitis Fundamentals and Clinical Practice: Fourth edition. Mosby Elsevier, 2010:51-58.
2. Jabs DA, Nussenblatt RB, Rosenbaum JT. Standardization of Uveitis Nomenclature (SUN) Working Group. Standardization of nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol. 2005;140:3:511.




