 |
Bios Dr. Fortenbach is an DISCLOSURES: The authors have no relevant disclosures. |
A 44-year-old woman with von Hippel-Lindau syndrome presented for follow-up with the ocular oncology service at the University of Washington Medicine Eye Institute. She has a history of two peripheral retinal capillary hemangioblastomas (RCHs) in the left eye and has previously undergone successful laser photocoagulation of these vascular tumors. She also has a history of juxtapapillary RCHs in both eyes. Half-fluence photodynamic therapy was trialed for the left juxtapapillary RCH five years prior to presentation with minimal response. Since then, the juxtapapillary tumors in both eyes have been monitored without treatment. At follow-up, the patient denied a change in vision.
Examination and Findings
Best corrected visual acuity was 20/20 in both eyes. Her pupils were equal and reactive without a relative afferent pupillary defect. Intraocular pressures were within normal limits in each eye. Dilated fundus examination revealed interval growth of the juxtapapillary RCH in the right eye compared to one year prior. The juxtapapillary RCH in the left eye was stable.
Imaging and Workup
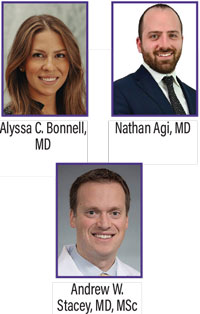
Optos fundus photography and fluorescein angiography demonstrated the juxtapapillary vascular tumors in both eyes
(Figure 1). The patient is also followed closely by the neurosurgery and urology services for monitoring and treatment of her central nervous system and renal tumors.
Management
Given the growth of the right juxtapapillary tumor, this case was discussed with the medical oncology service for consideration of belzutifan treatment. Belzutifan is a hypoxia-inducible factor 2-alpha (HIF-2α) inhibitor medication that was approved by the U.S. Food and Drug Administration in 2021 for the treatment of CNS, neuro-endocrine and renal tumors associated with von Hippel-Lindau syndrome.1 It’s an oral medication taken daily.1 It’s generally well-tolerated by most patients. Common side effects of the medication include anemia, fatigue, headache and nausea.1 After discussing the potential risks and benefits of therapy, the patient elected to trial belzutifan treatment.
 |
|
Figure 1. Optos fundus photography (A) and fluorescein angiography (B) of the juxtapapillary RCHs in both eyes at presentation. Follow-up Optos fundus photography (C) three months after starting belzutifan. |
Follow-up
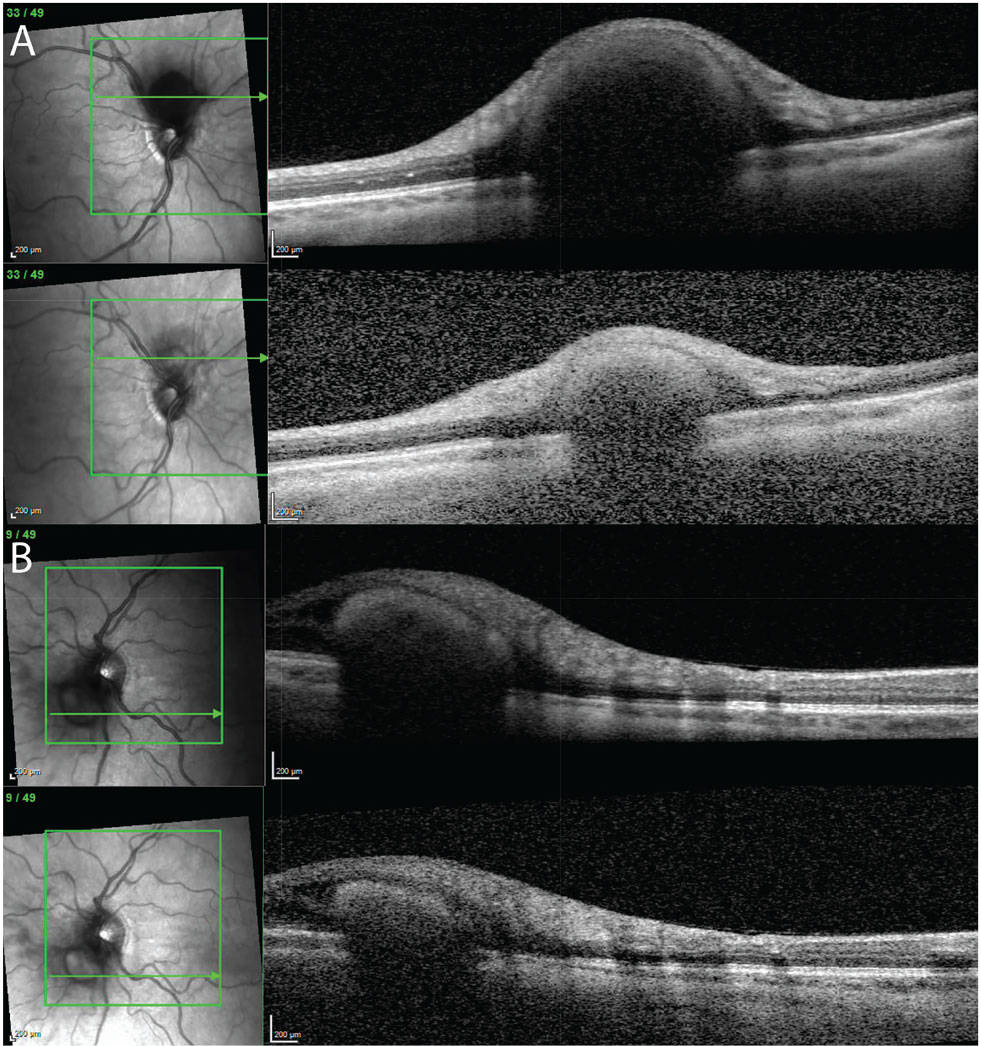
The patient followed up with the ophthalmology service three months after starting belzutifan. At follow-up, there was notable regression of the juxtapapillary tumors in both eyes (Figure 1 and Figure 2). She was tolerating the medication well.
Von Hippel-Lindau Syndrome
Von Hippel-Lindau syndrome is a rare, autosomal dominant disease characterized by many systemic tumors, including retinal and CNS hemangioblastomas, pheochromocytomas and clear cell renal carcinomas.2 These tumors form due to a mutation or loss of the VHL tumor suppressor gene on chromosome 3.2
Ophthalmologists are often the first specialists to diagnose patients with von Hippel-Lindau syndrome because retinal capillary hemangioblastomas are most commonly the first presenting sign of disease, followed by central nervous system hemangioblastomas.3 The lifetime risk of developing RCHs for all patients with von Hippel-Lindau syndrome is about 70 percent.3 The average age of onset of retinal capillary hemangioblastomas is 25 years.3
Close surveillance of patients is essential to reduce morbidity and mortality in this patient population, including vision loss. Renal cell carcinoma is the most common cause of mortality for patients.2
Retinal Capillary Hemangioblastomas
RCHs can be diagnosed and monitored through dilated fundoscopic examination of the retina and widefield imaging, including widefield fluorescein angiography. While small peripheral vascular tumors may be asymptomatic, tumors with exudation affecting the macula can lead to vision loss.4 Less common sequelae of these retinal tumors include neovascularization leading to vitreous hemorrhage and glaucoma, large exudative retinal detachment, or tractional retinal detachment due to glial cell proliferation on the retinal surface.4
Ablative therapy is preferred for extrapapillary and extramacular vascular tumors. Tumors smaller than 1.5 mm can often be effectively treated with laser photocoagulation.4 Larger tumors may require other ablative modalities, such as cryotherapy or brachytherapy. Rarely, with advanced disease, vitreoretinal surgery may be indicated.
 |
|
Figure 2. Optical coherence tomography imaging of the juxtapapillary tumors at baseline (top) and three months after initiating daily belzutifan treatment (bottom) in the (A) right and (B) left eyes. |
Juxtapapillary and Macular Tumors
Treatment for juxtapapillary and macular RCHs is particularly challenging. In these cases, ablative therapy may lead to permanent vision loss. Full- or half-fluence PDT has been reported to be successful in some cases, but it was unsuccessful for our patient.5
A New Treatment: Belzutifan
Belzutifan is a novel HIF-2α inhibitor taken as an oral medication.1 The dose is 120 mg daily.1 This report and others have demonstrated regression of RCHs with belzutifan use.6-9 This medication may be most beneficial for juxtapapillary or macular tumors, where typical ablative treatment is challenging. Belzutifan may also be helpful in eyes with large peripheral tumors. Tumor regression with treatment may allow for greater success with laser photocoagulation, as opposed to more invasive and destructive treatments.
While belzutifan therapy is generally well-tolerated, about one-third of patients will discontinue the medication due to side effects, like fatigue.10 The potential for RCH recurrence after discontinuing treatment must be considered for these patients. Reduced medication dose to 80 mg daily has been reported to control the retinal tumors in one case with short-term follow-up.9
Bottom Line
Ophthalmologists are often the first specialists to diagnose von Hippel-Lindau syndrome. Prompt and appropriate referral for close systemic surveillance with appropriate subspecialists is essential. Common extraocular tumors include CNS hemangioblastomas, pheochromocytomas and renal cell carcinomas. Early treatment of RCHs may improve visual outcomes for patients. For challenging lesions near the optic nerve and macula, the novel HIF-2α inhibitor, belzutifan, may be an effective treatment. However, the potential for recurrence of these vascular tumors after discontinuation of treatment must be considered. RS
References
1. Jonasch Eric, Donskov Frede, Iliopoulos Othon, et al. Belzutifan for renal cell carcinoma in von Hippel–Lindau Disease. N Engl J Med. 2021;385:22:2036-2046.
2. van Leeuwaarde RS, Ahmad S, van Nesselrooij B, Zandee W, Giles RH. Von Hippel-Lindau syndrome. In: Adam MP, Feldman J, Mirzaa GM, et al., eds. GeneReviews. Seattle: University of Washington, 1993. Accessed May 27, 2024.
3. Maher ER, Yates JR, Harries R, et al. Clinical features and natural history of von Hippel-Lindau disease. Q J Med. 1990;77:283:1151-1163.
4. Singh AD, Nouri M, Shields CL, Shields JA, Perez N. Treatment of retinal capillary hemangioma. Ophthalmology. 2002;109:10:1799-1806.
5. Papastefanou VP, Pilli S, Stinghe A, Lotery AJ, Cohen VML. Photodynamic therapy for retinal capillary hemangioma. Eye. 2013;27:3:438-442.
6. Cotton CC, Chandrabhatla AS, Andrews PH, Purrow BW, Shildkrot YE. Belzutifan for treatment of giant retinal hemangioblastoma with extrascleral extension associated with von Hippel-Lindau syndrome. Retin Cases Brief Rep. November 7, 2023. (Online publication).
7. Ercanbrack CW, Elhusseiny AM, Sanders RN, Santos Horta E, Uwaydat SH. Belzutifan-induced regression of retinal capillary hemangioblastoma: A case-series. Am J Ophthalmol Case Rep. 2024;33:102011.
8. Jones AA, Schloemer NJ, Wirostko WJ. Successful Treatment of Von Hippel-Lindau (VHL) Disease-associated retinal capillary hemangioblastoma (RCH) with Belzutifan in a pediatric patient. Retin Cases Brief Rep. July 13, 2023 (online publication).
9. Ercanbrack CW, Elhusseiny AM, Sanders RN, Horta ES, Uwaydat SH. Case Reports. Belzutifan-induced regression of retinal capillary hemangioblastoma: A case-series. Am J Ophthalmol Case Rep 2024:10:33:102011.
10. Courtney KD, Ma Y, Diaz de Leon A, et al. HIF-2 complex dissociation, target inhibition, and acquired resistance with PT2385, a first-in-class HIF-2 inhibitor, in patients with clear cell renal cell carcinoma. Clin Cancer Res. 2020;26:4:793-803.



